Peláez Pérez JM (1), Sánchez Casado M (2), Quintana Díaz M (3).
(1) MD, Anesthesia, Toledo Hospital Complex, Toledo, Spain
(2) PH, MD Intensiv Care specialist, La Paz Universitary Hospital, Madrid, Spain
(3) PH, MD Intensiv Care specialist, Toledo Hospital Complex, Toledo, Spain
Introduction
Since the development of «hypnosedation» by anaesthesiologist Faymonville et al. in 1977(1), the combination of hypnosis and conscious sedation techniques with low-dose intravenous drugs, or local or locoregional anaesthetic infiltration, has demonstrated multiple advantages. These advantages have been observed both in the preoperative phase, given the correlation between preoperative anxiety and postoperative pain (2, 3), in the perioperative phase, with efficacy observed in minimally invasive procedures and awake craniotomy(4, 5), and in the postoperative phase, with evidence of a reduction in nausea and vomiting, pain and early awakening and discharge(6, 7).
Better knowledge of the technique and its greater use in operating theatres has led to the abandonment of the concept of sedation in favour of that of analgesia, which is why the term hypnoanalgesia is now used instead of hypnosedation. Patients treated under hypnosis show greater comfort and lower levels of anxiety(8, 9). In addition, the high receptivity and suggestion reached with hypnosis during anaesthesia help to reduce analgesic and sedative doses during and after the surgical procedure, which facilitates recovery(10, 11).
Doctors and surgeons in the early 19th century already pointed out that children and adolescents were particularly «sensitive» to hypnotic techniques, showing good response to hypnotherapeutic strategies(12). However, most studies of hypnosis and pain have been conducted in adults. The mechanisms of action proposed for non-pharmacological comprehensive therapies in adults may differ in the paediatric population due to, among other reasons, possible developmental effects, requiring specific studies in that population(10, 13-15).
The aim of this study was to assess whether the use of hypnoanalgesia in dermatological surgery in the paediatric population reduces the need for sedation and analgesia during the procedure, and its impact on pain in the immediate post-operative period and after 24 hours. Secondary objectives were to assess the degree of acceptance of the procedure and to evaluate the efficacy of the technique according to the age of the patients and, therefore, their suggestibilit.
Patients and Methods
Design
A 1:1 parallel group unicenter randomized clinical trial was conducted. The study was conducted in accordance with the WHO code of ethics (Declaration of Helsinki) on human experimentation and was approved by the Clinical Research Ethics Committee of the Toledo Hospital Complex.
Randomisation and masking
Randomisation was carried out in blocks, depending on the day of the operation (day with hypnosedation or day with distraction), without the dermatologists or the anaesthetist performing the operation having prior knowledge of either the assigned day or the «suggestibility» of the cases, respectively.
The blind was achieved by assigning different investigators to each phase of the study, with one designated as responsible for recruitment (MQD), another for intervention and control (JMPP), and another for subsequent evaluation in the post-anaesthesia recovery unit (URPA) and at 24 hours (responsible nursing staff).
Participants
Children scheduled for dermatological surgery were recruited for major outpatient surgery (MOS) at the National Paraplegic Centre. The following inclusion criteria were established: 1) A class I or II of anaesthetic risk according to the American Society of Anesthesiologists, 2) to be in a percentile between P3 and P97 in weight and height, 3) without known drug allergies, and 4) having fasted 6 hours for solids and 2 hours for water. Children with diagnosed mental retardation or attention deficit, behavioural disorders, previous treatment with hypnosis, history of neurological pathology or psychomotor retardation, previous pain-related pathology, or obstructive sleep apnoea syndrome (OSAS) were excluded. Recruitment was carried out by the principal investigator from the surgical waiting list for a period of 5 months (November 2017 to April 2018). All patients who met the inclusion criteria were given informed consent and an information sheet, both on the anaesthetic procedure and on hypnosis as an adjuvant technique.
Intervention, control and procedures
Patients were randomly distributed to one of the following groups:
Intervention group: A technique of rapid conversational hypnosis was used, with focus and therapeutic suggestion (guiding the patient into a hypnotic trance), adapted to the cognitive development. Induction with hypnotic suggestion focuses and accompanies the child’s body sensations and allows their active participation. After standard sedation, therapeutic suggestion is maintained throughout the surgery and in the post-hypnotic period before awakening.
Control group: A high-tech distraction technique (Apple®) was used, passive and chosen by the child, either an animated video or his or her favourite music. After standard intravenous sedation, the child was taken to the operating theatre to watch his or her favourite video or music and this was maintained throughout the procedure.
In the previous anaesthesia consultation, the therapeutic alliance was established with all the children, regardless of the group assigned, giving them the opportunity to choose their favourite experience of therapeutic suggestion, according to their age and level of cognitive maturity. Patients and tutors were given a behavioural therapeutic session to reduce the anxiety and fear associated with the procedure and to eliminate any negative connotations associated with medical hypnosis.
Prior to surgery, the pre-surgical checklist was completed. The entire surgical team had received training in conversational hypnosis and attention-distracting techniques from the principal investigator, a paediatric anaesthetist, with academic qualifications and experience in clinical hypnosis.
In the anteroom of the operating room, all children were offered to play, such as with fruit-smelling markers to colour the inside of the anaesthetic mask (Stabylo®).
During surgery, ¬¬standard sedation was performed either intravenously or inhalationally as an option. In the endovenous induction, an initial dose of propofol of 2.5 mg/Kg was injected, registering the additional amount needed. If the additional doses were not sufficient, a short duration opioid, alfentanil, was administered at a dose of 10-15 micrograms/kg. For inhalation induction, a mixture of nitrous oxide and oxygen (60/40) was administered at tidal volume with an external Mapelson C circuit (Maquet Flow-i C20®). Finally, the surgeon, in agreement with the anaesthetist, used local anaesthesia with 2% subcutaneous lidocaine.
Waking up was carried out in the operating theatre with subsequent transfer to the Post-Anaesthesia Care Unit (PACU), where, in addition to control of constants, pain was assessed using adapted scales (see variables and measurements below), and analgesics were administered where necessary (if VAS>4 paracetamol was used, 15 mg/kg, and if pain persisted, magnesium metamizole at a dose of 20 mg/kg).
Evaluation and Outcome Measures
The following outcome variables were established:
• Main variable: Total dose of propofol and additional need for opioids during the operation, measured in mg/kg of weight as recorded intra-operatively.
• Impact on pain and analgesic needs, both in the immediate post-operative period and 24 hours after the operation, measured by pain scales adapted to age and cognitive maturation (Visual Analogical Scale (VAS) from 10 years and Face Drawing Scale or FPS-r from 5 to 9 years), need for paracetamol, ibuprofen or other analgesics. The scales were given to the children by the nurse in charge at the PACU, who was also responsible for the 24-hour post-surgery follow-up, and did not know the group to which each patient belonged. The analgesic need was collected from the medical logs.
• Degree of satisfaction with the procedure, using a scale of 1 to 10, administered at the time of discharge from hospital to the children or their guardians.
Statistical analysis
For the descriptive analysis, central tendency and dispersion measures were used (median and 25th to 75th percentiles, P25-75) for quantitative variables, and absolute and relative frequencies for qualitative ones. The comparison of the outcome measures between the intervention group and the control group was carried out by means of non-parametric tests: chi-square and Fisher’s exact test for qualitative outcome measures, and Mann-Whitney’s U for the quantitative ones.
An age-based subgroup analysis was conducted (under 7 years and over).
The significance level was set at a value of p<0.05 and the analysis was carried out with Excel®.
A sample of 30 patients was calculated to detect a 40 mg dose difference between the two groups, with a risk α of 0.05 and a risk β of 0.20 in a bilateral contrast and assuming a common standard deviation of 33.3 and a loss to follow-up rate of 10%.
Results
From November 2017 to April 2018 a total of 30 patients were recruited, of which 28 met the selection criteria and were included in the trial, 15 randomised to hypnosis and 13 to control (Fig. 1). The two patients excluded were one due to having OSAS and another one to having attention deficit disorder. All the randomised patients completed the study. The indications for surgery were: nevus (n=15), local neoplasms (n=4), and other lesions (2 pilomatrixoma, 3 cysts, 1 angioma, 1 epidermiolysis bullosa, 1 plantar hyperhidrosis, 1 papillothrixoma and 1 trichoepithelioma). The ages were between 5 and 16 years, with 50% being 8 years old or younger. All were 28 kg or more in weight. There were no significant differences in the baseline characteristics of the patients between groups (Table 1).
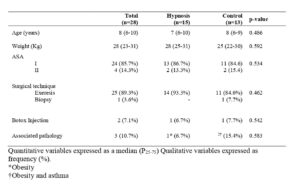
Table 2 shows the results in the three evaluation periods: during surgery, in the immediate post-operative period, and after 24 hours. Compared to the control group, patients undergoing surgery with hypnosis required lower doses of propofol intraoperatively, both in absolute value (50 vs 70 mg; p<0.001) and per kg of weight (1.78 vs 2.86; p=0.001), presented less pain in the Faces Pain Scale revised (FPS-r) at 24 hours (0 vs 3; p=0.019), and the duration of the stay in the PACU was shorter (60 vs 90 minutes; p=0.019).
Sixty percent of the patients required pain medication in the first 24 hours, the most common being paracetamol. No differences were observed between groups in the frequency of paracetamol use, but for ibuprofen it was necessary in fewer patients in the hypnosis group than in the control (6.7% vs 38.5%; p=0.041). For the remaining variables, the differences between groups did not achieve statistical significance, despite a clear difference in favour of the hypnosis group.
With regard to the analysis by age group, in both cases a trend towards better results was observed in all variables, regardless of the group, but statistically significant differences were only shown in the group of children over 7 years of age with regard to the need for intraoperative propofol (50 vs 80 mg), to post-operative pain measured by VAS (0 vs 5) and by the post-operative FPS-r scale (0 vs 5.5) and at 24 hours (0 vs 2.5) and in the need for ibuprofen at 24 hours (no child vs 5) (Table 3).
Regarding the satisfaction scale, globally the rating was high, 9 (8-9), with significant differences (p < 0.02) between the groups’ ratings: 8 (8-10) in the group without hypnosis and 9 (9-9) in the group with hypnosis. In the analysis by age no differences are found.
Finally, no complications or adverse effects were reported that could be attributed to hypnosis or distraction.
Discussion
The results of our study show a significant reduction in the intra-operative dose of propofol required, pain and need for ibuprofen after 24 hours, time in PACU and greater satisfaction with hypnosis compared to distraction techniques in children undergoing dermatological surgery.
The trial subjects represent a paediatric population over 5 years of age in which surgery is considered major, even if it is outpatient. There is sufficient variability in terms of age and indications for surgery, always within the dermatological criteria, so we believe that the results are of sufficient generalisability.
The French Association of Medical Hypnosis (AFHM) defines hypnosis as a relational experience between the patient and the doctor whose goal is the «perceptual modification» of an intended medical care(16). The hypnotic process modifies the activity of the cortical-subcortical, limbic and paralymbic brain areas, which are related to the sensory and cognitive perceptions of the stimulus, which have been characterised in neuroimaging techniques as the structures involved in the neuromatrix of pain(17).
According to the International Association for the Study of Pain (IASP), pain is «an unpleasant sensory and emotional experience associated, or similar to that associated, with actual or potential tissue damage». Pain is always a personal experience influenced by biological, psychological and social factors that can be expressed verbally or non-verbally and whose adaptive function can have adverse effects on social and psychological function and well-being. Pain and nociception are different phenomena(18). Therefore, pain is more complex than a stimulus-response action. The painful experience is initiated and maintained in specific brain structures and its end result is determined by memory, cognitive status and emotional situation.
Hypnosis is a non-pharmacological intervention that has been shown to modulate pain intensity and perception at the supra-spinal level, in the so-called neuromatrix of pain18. Studies by Montgomery et al. on invasive surgical procedures have shown that hypnosis effectively controls pain and stress, facilitates recovery, and provides targeted medical care with actions at different levels(19, 20). In addition to mobilising internal resources through suggestion, hypnosis also modifies the perception of pain or suffering by shifting attention, and creates a virtual imaginary that promotes positive attitudes and greater adherence to medical indications. Other effects are related to improving coping skills, respecting patient autonomy, promoting therapeutic education, and preventing further medical care.
Pain, anxiety in the surgical setting, and the need for adjuvant treatment used synergistically to complement drug therapy are clearly established in the scientific literature, although previous studies with hypnosis showed contradictory results(21). Our study, which focused on analgesia rather than anxiety, supports the use of hypnotherapeutic techniques in outpatient surgery. In general, pain levels experienced by children in our trial were not very high, in fact at 24 hours 50% in both groups reported a VAS of 0. Even so, and also given the small sample size, the results confirm the experience in adults of the usefulness of hypnosis as a co-adjuvant to anaesthesia in reducing pain caused by surgery. The reduced need for analgesia with ibuprofen in patients who received hypnosis confirms that the painful process is subject to neuromodulation, increasing or decreasing proportionally from the beginning of the process. For this reason, non-pharmacological adjuvant techniques, such as hypnosis, which favour patient comfort, would prolong their action beyond the surgical procedure and the immediate post-operative period. All these findings explain the overall greater satisfaction with the procedure in the hypnosis group. Multimodal analgesia combines pharmacological and non-pharmacological interventions, with additive or synergistic effects, and is the most effective treatment for pain relief compared to single-modality interventions, also achieving an improvement in the patient’s quality of life and well-being(22).
In terms of performing a subanalysis by age group, our hypothesis was that in the subgroup of patients under 7 years of age the usefulness of hypnosis would be greater than in older children. This is due to a greater suggestibility when compared to hypnosedation with great ease to enter into a trance as their critical thinking is not developed23. However, although there were clear differences in the younger group between hypnosis and control, we could not detect statistically significant differences, clearly in relation to the small statistical power after stratification.
Among the limitations of this study are those inherent to the very nature of the hypnosis process that requires the collaboration of the patient, which makes it difficult to meet the standards of a randomised, double-blind, controlled clinical trial. In this trial there was only one person performing the hypnosis and control techniques, which can be seen as a potential bias. To reduce the possible associated bias, a previous trial was conducted with the same methodology and training of the surgical team in conversational hypnosis and the study was blinded to post-intervention medical care providers. In addition, families were warned that the children would be distracted by different techniques, but the exact technique, whether it was hypnosis or not, was not disclosed, and so the children did not know if they were receiving hypnosis or distraction, only ‘techniques’. In fact, the level of satisfaction with the control techniques was also very high.
Another limitation of this trial is the small sample size for subgroup analysis and specific outcomes, not only the main endpoint. The results obtained in favour of the hypnosis group are important, especially in terms of reduction of intra- and post-operative medication, satisfaction and recovery time in the PACU and 24 hours after the intervention, all of which should result in less toxicity, less use of resources and more collaboration in the recovery.
In conclusion, the results of this trial, taking into account its limitations, support the safe use of hypnosis by trained personnel in paediatric outpatient surgical settings in order to improve perioperative pain perception, as an adjuvant to sedation.
References
- Faymonville ME, Mambourg PH, Joris J, Vrijens B, Fissette J, Albert A, et al. Psychological approaches during conscious sedation. Hypnosis versus stress reducing strategies: a prospective randomized study. Pain. 1997;73:361-7.
https://doi.org/10.1016/s0304-3959(97)00122-x - Duparc-Alegria N, Tiberghien K, Abdoul H, Dahmani S, Alberti C, Thiollier AF. Assessment of a short hypnosis in a paediatric operating room in reducing postoperative pain and anxiety: A randomised study. J Clin Nurs. 2018;27:86-91.
https://doi.org/10.1111/jocn.13848 - Fortier MA, Weinberg M, Vitulano LA, Chorney JM, Martin SR, Kain ZN. Effects of therapeutic suggestion in children undergoing general anesthesia: a randomized controlled trial. Paediatr Anaesth. 2010;20:90-9.
https://doi.org/10.1111/j.1460-9592.2009.03225.x - Miller K, Tan X, Hobson AD, Khan A, Ziviani J, O’Brien E, et al. A Prospective Randomized Controlled Trial of Nonpharmacological Pain Management During Intravenous Cannulation in a Pediatric Emergency Department. Pediatr Emerg Care. 2016;32:444-51.
https://doi.org/10.1097/PEC.0000000000000778 - Lohkamp LN, Mottolese C, Szathmari A, Huguet L, Beuriat PA, Christofori I, et al. Awake brain surgery in children-review of the literature and state-of-the-art. Childs Nerv Syst. 2019;35:2071-7.
https://doi.org/10.1007/s00381-019-04279-w - Browne PD, den Hollander B, Speksnijder EM, van Wering HM, Tjon ATW, George EK, et al. Gut-directed hypnotherapy versus standard medical treatment for nausea in children with functional nausea or functional dyspepsia: protocol of a multicentre randomised trial. BMJ Open. 2019;9:e024903.
https://doi.org/10.1136/bmjopen-2018-024903 - Calipel S, Lucas-Polomeni MM, Wodey E, Ecoffey C. Premedication in children: hypnosis versus midazolam. Paediatr Anaesth. 2005;15:275-81.
https://doi.org/10.1111/j.1460-9592.2004.01514.x - Lynn SJ, Kirsch I, Barabasz A, Cardena E, Patterson D. Hypnosis as an empirically supported clinical intervention: the state of the evidence and a look to the future. Int J Clin Exp Hypn. 2000;48:239-59.
https://doi.org/10.1080/00207140008410050 - Pelaez-Perez JM. Entrée dans l’IRM. Le tunnel magique et filin. Revue Hypnose & Thérapies brèves. 2019:50-2.
- Kuttner L. Pediatric hypnosis: pre-, peri-, and post-anesthesia. Paediatr Anaesth. 2012;22:573-7.
https://doi.org/10.1111/j.1460-9592.2012.03860.x - Mackey EF. An Extension Study Using Hypnotic Suggestion as an Adjunct to Intravenous Sedation. Am J Clin Hypn. 2018;60:378-85.
https://doi.org/10.1080/00029157.2017.1416279 - Oleness K, Kohen DP. Hypnosis and Hypnotherapy with children. 4th ed. New York: Guillford; 1996.
- Richardson J, Smith JE, McCall G, Pilkington K. Hypnosis for procedure-related pain and distress in pediatric cancer patients: a systematic review of effectiveness and methodology related to hypnosis interventions. J Pain Symptom Manage. 2006;31:70-84.
https://doi.org/10.1016/j.jpainsymman.2005.06.010 - Wood C, Bioy A. Hypnosis and pain in children. J Pain Symptom Manage. 2008;35:437-46.
https://doi.org/10.1016/j.jpainsymman.2007.05.009 - Faymonville ME, Laureys S, Degueldre C, DelFiore G, Luxen A, Franck G, et al. Neural mechanisms of antinociceptive effects of hypnosis. Anesthesiology. 2000;92:1257-67.
https://doi.org/10.1097/00000542-200005000-00013 - Tosti G. Definitions et rouages de l’hypnosis. In: Eyrolles G, editor. Le grand livre de l’hypnose. Paris2016. p. 38-40.
- Vanhaudenhuyse A, Boly M, Balteau E, Schnakers C, Moonen G, Luxen A, et al. Pain and non-pain processing during hypnosis: a thulium-YAG event-related fMRI study. Neuroimage. 2009;47:1047-54.
https://doi.org/10.1016/j.neuroimage.2009.05.031 - Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, et al. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain. 2020.
https://doi.org/10.1097/j.pain.0000000000001939 - Montgomery GH, DuHamel KN, Redd WH. A meta-analysis of hypnotically induced analgesia: how effective is hypnosis? Int J Clin Exp Hypn. 2000;48:138-53.
https://doi.org/10.1080/00207140008410045 - Montgomery GH, Schnur JB, Kravits K. Hypnosis for cancer care: over 200 years young. CA Cancer J Clin. 2013;63:31-44.
https://doi.org/10.3322/caac.21165 - Manyande A, Cyna AM, Yip P, Chooi C, Middleton P. Non-pharmacological interventions for assisting the induction of anaesthesia in children. Cochrane Database Syst Rev. 2015:Cd006447.
https://doi.org/10.1002/14651858.CD006447.pub3 - Friedrichsdorf SJ. Multimodal pediatric pain management (part 2). Pain Manag. 2017;7:161-6.
https://doi.org/10.2217/pmt-2016-0051 - Thompson T, Terhune DB, Oram C, Sharangparni J, Rouf R, Solmi M, et al. The effectiveness of hypnosis for pain relief: A systematic review and meta-analysis of 85 controlled experimental trials. Neurosci Biobehav Rev. 2019;99:298-310.
https://doi.org/10.1016/j.neubiorev.2019.02.013






Artículo novedoso, muy interesante y que abre un campo de lo más prometedor en la atención pediatrica. Enhorabuena a la autora.
Un artículo muy interesante que aporta luz sobre un tema desconocido para muchos de nosotros, enhorabuena a la autora
Muy interesante
Mis felicitaciones por este gran trabajo que nos abre a un campo tan interesante como la hypnoanalgesía.